Tongue and Lip Ties
If you think your child may be experiencing symptoms due to a tongue or lip tie, call to schedule an appointment today!
Why is it important to diagnose and treat tongue and lip ties?
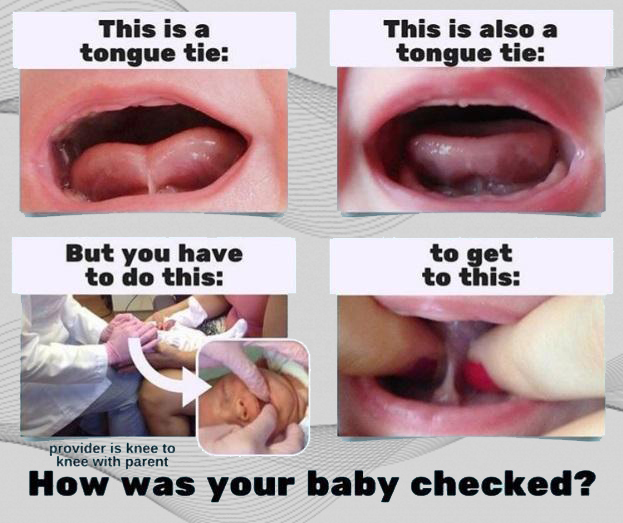
Unfortunately, physicians and dentists are not specially trained in school on how to properly examine babies for tongue ties. Without proper techniques and knowledge, it is easy to arrive at the conclusion that a tongue tie is not present or interfering in the breastfeeding process – when in fact, it is. Tongue ties go beyond feeding issues and are an overall health concern.
Why we treat it
Babies will nurse better and have better growth and development. Later in life it can mean less issues with or prevention of speech issues, gagging, breathing issues and TMD. see more
Not only will babies be able to nurse, or nurse better (less gas and reflux), they will also have a better chance at developing properly. We know form follows function. The palate will only get that nice “horse shoe” shape if the tongue is able to go up there during swallowing and play. If it can’t go there, the palate will begin to collapse on the sides resulting in a high, narrow palate. When this happens the lower jaw follows. This can result in crowding issues in the baby and permanent teeth. The tongue not being able to lift up to the roof of the mouth means that it is down and back. This can cause airway issues early and throughout life such as snoring and/or mouth breathing.
Also, the tongue is a stabilizer. Bringing it to the roof of the mouth gives babies and adults the sense of stability and releases oxytocin. Without this they may tend to grind their teeth or have other core/stability issues.
It can result in speech issues, gagging, breathing issues, TMD issues all later in life.
Signs of a Tongue/Lip Tie besides seeing the actual tie
Click on each one for a more detailed explanation
an unstimulated palate often results in excessive gagging in infants and adults too. This is because if that area of the mouth was constantly being stimulated by a proper tongue habit, it would be desensitized. If the tongue does not/cannot go there, it will by hypersensitive and result in gagging
reflux, poor latch, long feedings, baby getting tired/sweaty during feedings, poor weight gain all can be associated with a tongue tie
A poor/shallow latch causes nipple damage which can become infected with bacteria or fungus
babies want oxytocin from stimulating the palate, if they can’t get it with the tongue they will get it another way
estimates say that 90% of people with a lip tie will also have a tongue tie
especially around the upper teeth. If a tie is present, it makes clearing of milk and food more difficult. A child may keep milk or food in these areas longer than they should.
The tongue is the main stabilizing muscle and without it children and adults will use their teeth for stability instead-grinding can be caused by other issues as well
When to treat
Infants should be treated when there is a noted restriction that is causing symptoms. Usually, frenums (or attachments of soft tissue) are present for a reason, but when there is a restriction with symptoms it should be treated as soon as identified. Ideally this would be in the first few weeks of life. Assessing them can be tricky especially for posterior tongue ties. In fact, many pediatricians, lactation specialists and ENTs do not know how to properly assess them. To assess them properly, you need to put your fingers on either side of the tongue and lift and feel/look for restriction. So if the tip is tied, many practitioners can identify this and will recommend treatment. But if it isn’t that’s is where many practitioners stop and say “its not a tie”. Remember, it’s the middle portion of the tongue that has to get to the palate. The posterior tie is what eludes many practitioners but it is like sail boat and its mast. A Class I tie is like the sailboat at full mast. Large wide, easy to see. The Class IV is if the sail is all the way down. There is just a mast, narrow, thin, but it’s there and can cause tongue dysfunction. Lips are assessed by lifting and trying cover the nostrils. If it blanches, or turns any tissue white, it may be a restriction. see more
How we treat
We use a laser or sometimes combination of scissors and laser. The laser is very nice because it cauterizes and stimulates healing so there is little bleeding and virtually no risk of infection as well as less pain. We do not sedate. We swaddle for children under 1 years of age. We use a topical numbing agent appropriate for the age of the patient so that it can be swallowed with no side effects. The procedure usually takes about 5 minutes total. The children under 1 often cry the entire procedure beginning with the numbing medication. The procedure on the pain scale is considered “mild to moderate” and most children are done crying as soon as we unswaddle them. For the first 12-24 hours they may be a little fussy or refuse to eat/not eat well but they are usually back to themselves within 24 hours of the procedure. see more
Aftercare
The wound will look like a white diamond after the procedure and it may bleed a little for a few days. We want the would to heal open and not seal back down. So parents or patients will need to make swipes in the treated area several times a day to make sure it doesn’t heal down. Six times a day is the recommended amount. We recommend Tylenol or Advil as needed for the first day or two but they usually don’t need it or only need it the same day.see more
Follow-up THE BIGGEST KEY TO SUCCESS
Any release on an infant or child should be followed up with a team approach. They need to re-learn and retrain. Remember, they have been swallowing and developing their palate/tongue position since 18 week in utero. So a one week old doesn’t have a one week old habit/pattern. Just because it’s no longer restricted, doesn’t mean they’ll know what to do. So this means follow-up with a well trained lactation consultant to re-train and relearn a good latch for nursing children. Older kids and adults should be seeing someone trained in orofacial myology. These are people specifically trained in the function of the tongue. Some speech language pathologists and/or dental hygienists may have this special training. There are only 2 in our area that I am aware of.